Understanding Lung Cancer: A Comprehensive Guide to Check for Lung Cancer
Lung cancer is a leading cause of cancer-related mortality around the globe. As with many diseases, early detection significantly improves treatment outcomes. This article aims to provide an in-depth understanding of how to check for lung cancer, the available diagnostic methods, and the importance of regular screening, especially for those at higher risk.
The Importance of Early Detection
Early detection of lung cancer can be pivotal in increasing survival rates. Studies have shown that patients diagnosed at an early stage have a significantly better prognosis. Therefore, understanding how to detect these critical signs and the relevant procedures to follow can save lives.
Why Check for Lung Cancer?
Lung cancer symptoms may not be apparent until the disease has progressed. Hence, regular screenings can help in catching the disease early. Additionally, knowing your risk factors can guide your decision to get screened. If you are a smoker, have a family history of lung cancer, or have been exposed to carcinogens, you should consider screening tests more seriously.
Common Symptoms of Lung Cancer
Before discussing how to check for lung cancer, it is essential to recognize the symptoms that may warrant a visit to your healthcare provider:
- Persistent Cough: A cough that doesn’t go away or worsens over time.
- Chest Pain: Discomfort or pain in the chest area during deep breaths, coughing, or laughing.
- Shortness of Breath: Experiencing a sudden or gradual increase in shortness of breath.
- Weight Loss: Unexplained weight loss can be a significant indicator of cancer.
- Fatigue: Constant exhaustion that doesn’t improve with rest.
- Wheezing: An audible wheeze when breathing can indicate obstruction or irritation.
Methods to Check for Lung Cancer
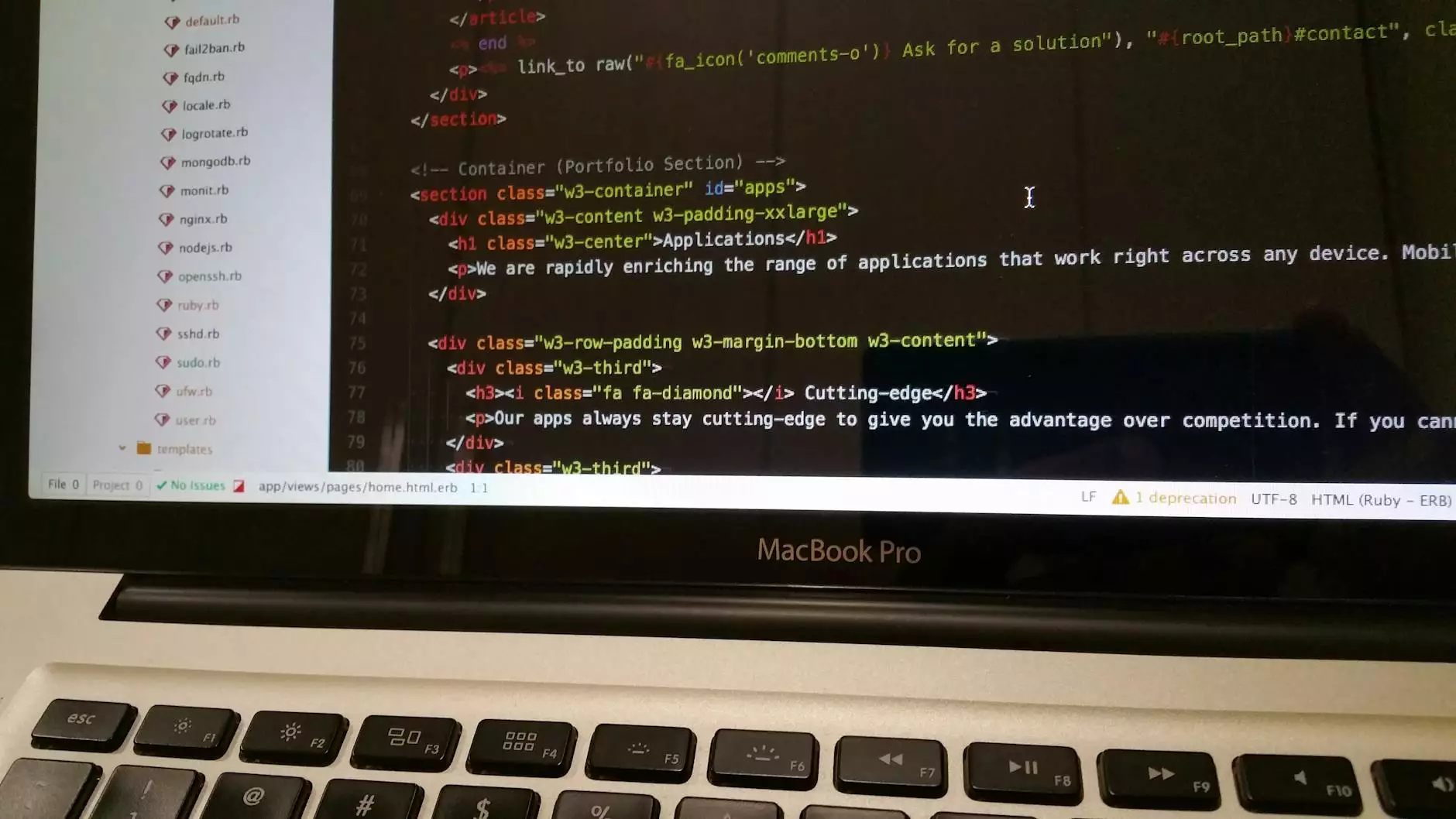
1. Medical Imaging: The First Step in Lung Cancer Detection
Medical imaging plays a crucial role in the preliminary diagnosis of lung cancer. Various imaging technologies are available, including:
- X-rays: A common first step that may show abnormal masses.
- CT Scans: More detailed than X-rays and can provide cross-sectional images of the lungs, assisting in identifying smaller tumors.
- MRI Scans: While not standard for lung cancer detection, MRIs can help in assessing if cancer has spread from the lungs to nearby structures.
2. Sputum Cytology: Analyzing Mucous
This test examines the mucus that you cough up. If lung cancer is present, cancerous cells may be detected in sputum. This method is non-invasive and can aid in the verification of an abnormality discovered through imaging.
3. Biopsy: The Definitive Test for Lung Cancer
A biopsy involves taking a sample of lung tissue to check for cancer cells. There are various biopsy methods, including:
- Transthoracic Needle Biopsy: A needle is inserted through the skin into the lung to obtain a tissue sample.
- Bronchoscopy: A procedure using a thin tube with a camera to look inside the lungs and obtain tissue samples.
- Thoracentesis: Involves collecting fluid from the pleural space around the lungs for analysis.
4. Molecular Testing: Targeting Cancer at the Genetic Level
Molecular testing identifies specific mutations in cancer cells that are crucial for determining targeted therapies. Patients with non-small cell lung cancer (NSCLC) might benefit from treatments tailored to specific genetic changes.
Screening Recommendations
According to health experts, specific groups may benefit from routine lung cancer screenings:
- Adults aged 50 years or older with a significant smoking history, defined as a 20-pack-year smoking history.
- Individuals who have quit smoking within the last 15 years and fall within the above age and smoking criteria.
Low-Dose CT Scan (LDCT)
The low-dose CT scan is recommended as a primary screening tool for lung cancer. This exam uses low levels of radiation to detect lung abnormalities while minimizing exposure. It has been shown to reduce mortality rates by aiding in the early detection of lung cancer.
Risk Factors for Lung Cancer
Understanding the risk factors can guide the decision on when and how to check for lung cancer:
- Smoking: The leading cause of lung cancer, accounting for approximately 85% of cases.
- Secondhand Smoke: Non-smokers exposed to secondhand smoke are also at increased risk.
- Occupational Hazards: Inhalation of substances like asbestos, arsenic, and diesel exhaust can increase risk levels.
- Genetic Factors: A family history of lung cancer can heighten an individual’s predisposition to the disease.
- Previous Lung Diseases: History of chronic lung diseases like COPD can potentially raise risk.
Current Advancements in Lung Cancer Detection
Ongoing research and technology developments in lung cancer detection are promising. Some noteworthy advancements include:
1. Artificial Intelligence in Radiology
AI is transforming how we interpret imaging studies. By using algorithms to analyze X-rays and CT scans, AI can potentially enhance the accuracy of lung cancer diagnosis and enable earlier detection.
2. Liquid Biopsies
Liquid biopsies analyze circulating tumor DNA from a blood sample. This non-invasive method holds the potential to uncover lung cancer earlier compared to traditional procedures.
Understanding Treatment Options
If lung cancer is detected, several treatment options are available, and these can vary based on the type and stage of cancer:
- Surgery: Often the first line of treatment for localized lung cancer.
- Radiation Therapy: Frequently used for tumor control or palliation.
- Chemotherapy: Systemic treatment that may be used at various stages of lung cancer.
- Targeted Therapy: Uses drugs or other substances to precisely identify and attack cancer cells.
Conclusion
In conclusion, understanding how to check for lung cancer is crucial for anyone at risk. Through awareness of symptoms, regular screenings, and advancements in medical technology, the fight against lung cancer can be strengthened. Staying informed and vigilant about lung health can lead to early interventions that save lives.
For those considering screening, particularly high-risk individuals, it is advisable to consult with a qualified healthcare provider. Early detection could mean the difference between life and death.
For more information and resources, visit Neumark Surgery